Click play for an audio readthrough of this article
Perimenopause – most of us know some of its physical symptoms, but what about the mental?
Menopause is the umbrella term for this lifestage and it actually breaks into three distinct phases: perimenopause, menopause and postmenopause. Perimenopause comes first and it’s the phase associated with symptoms – hot flushes, night sweats, brain fog, insomnia and so on.
Some people may be familiar with the physical symptoms of perimenopause, but that’s much less the case for mental health symptoms.
In fact, mental health symptoms can be some of the earliest warning signs that perimenopause is pending. More than that, some of the most debilitating symptoms of perimenopause can be mental and emotional ones.
Women are seemingly much more willing to visit a GP when physical symptoms flare up, but we tend to tolerate things like low mood, anxiety, irritability, and tearfulness for much longer before seeking help. Emotional symptoms – we’d rather blame our stressful lives, roll up our sleeves and crack on.
But it’s so important to acknowledge these feelings and seek answers promptly. Too many women suffer too much for too long and it doesn’t have to be that way.
Warning, the following section contains talk of suicide.
If you or someone you know require urgent help and support please reach out to one or more of these organisations:
The Samaritans. Volunteers listen in confidence to anyone in any type of emotional distress, without judging or telling people what to do. Click here or call 08457 90 90 90.
Together All. This is a safe, online community where people support each other anonymously to improve mental health and wellbeing. Click here.
Mind. If you or someone you know if going through a difficult time, Mind can offer support with different mental health problems. Mind also offer specific support in mental health in sport. Click here or call 0300 123 3393.
Shout. This is the UK’s 24/7 crisis text service for adults and children requiring mental health support. Click here or text 85258.
Papyrus. Papyrus UK offer suicide prevention advice. Click here or call 0800 068 4141.
Did you know?
- Approximately 18% of women in early perimenopause and 38% of women in late perimenopause will experience symptoms of depression.
- Symptoms of anxiety appear to be more common leading up to perimenopause.
- According to the Office of National Statistics, the UK’s highest rate of female suicide* is among 50 – 54 year olds.
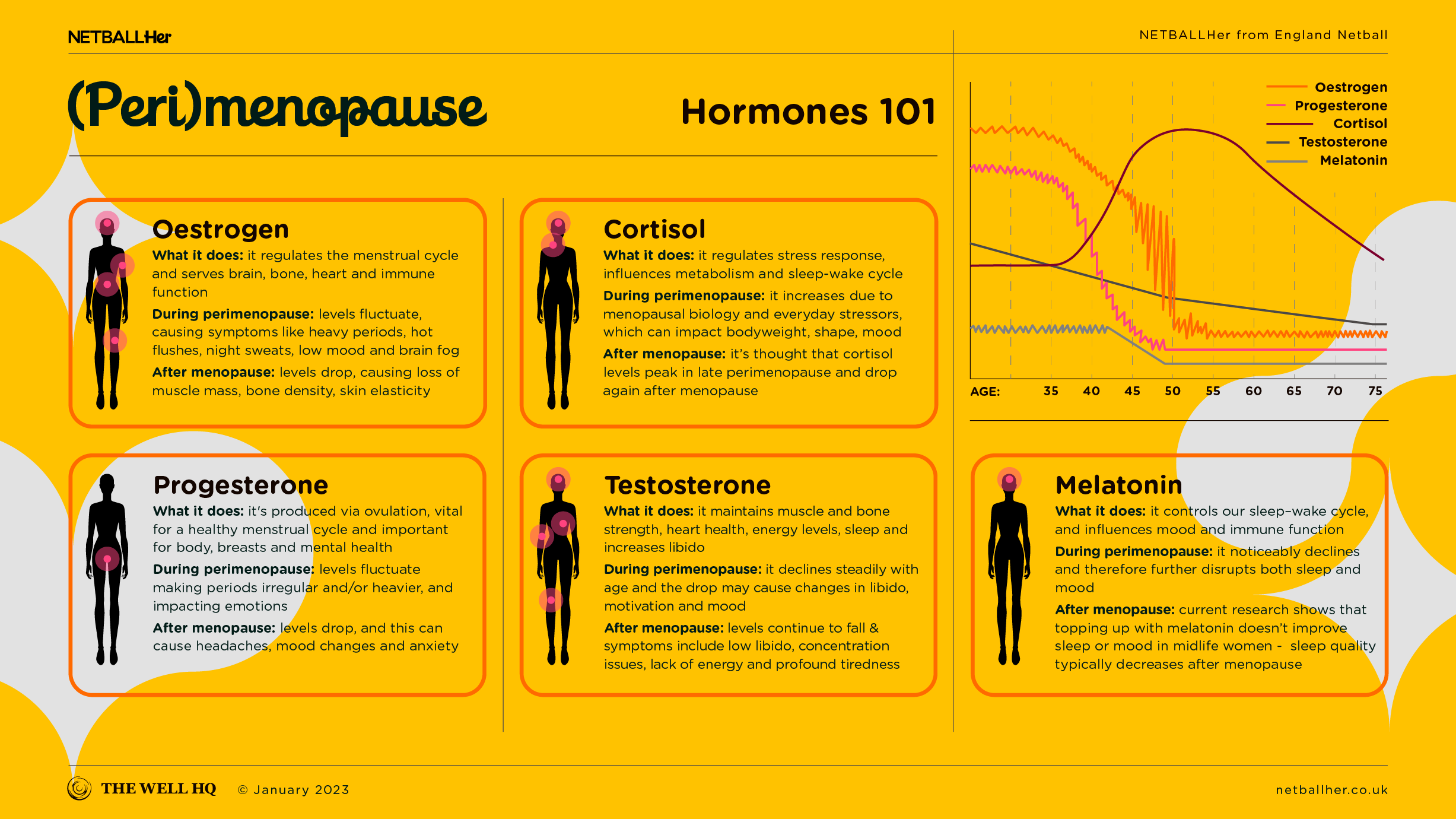
Oestrogen and mental health
A quick recap, oestrogen is one of the key female hormones. Women have oestrogen receptors in pretty much every cell of their body, including the brain, and oestrogen therefore plays a crucial role in cognitive function. In decision-making, resilience, mood regulation and so on.
Oestrogen winds down during menopause and that transition can rob women of their normal. The abrupt reduction in oestrogen invariably results in mental and emotional volatility – which can last for weeks, months or longer.
It’s worth noting that anxiety and depression are, of course, not exclusive to perimenopause nor are they guaranteed in perimenopause. Symptoms can run parallel. Not all women experiencing emotional turmoil are in menopause, and not all women in menopause will experience emotional turmoil. If in doubt see a doctor.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) is one avenue for potentially alleviating menopause-related mental health issues. HRT is now first-line treatment (as per NICE – the National Institute for Health and Care Excellence; the UK body in charge of setting guidance in clinical care) and something most women can consider using.
There are short and long term benefits to HRT but we always need to emphasise that not everyone needs it, wants it, or can have it. Prescription depends on individual risk factors, symptoms and medical history (women who’ve had oestrogen receptive breast cancer can’t have HRT, for example).
When it comes to hormone health and mental wellbeing, it’s important to remember there’s a complex relationship between HRT, perimenopausal symptoms and lifestyle factors such as diet, exercise and sleep. We therefore suggest you explore all your options with your doctor.
Exercise & movement
Exercise and movement are always our go-to when recommending positive, life-changing daily habits. They go such a long way to boosting how we think and how we feel.
Exercise releases endorphins and is proven to promote a greater sense of wellbeing. It reduces symptoms of anxiety and depression. Physical activity supports hormone regulation and, in turn, that helps to alleviate mood swings and irritability.
The more we discuss the impacts of menopause on our mental health, and how movement plays its part in the solution, the more we can support one another through life challenges. In netball, we have a ready-made environment to lean into for positivity and support. The more we discuss the psychological dimension of menopause, and how movement plays its part in the solution, the more we can support one another through life challenges such as menopause.
Knowledge (really) is power
Often, the act of simply acknowledging how challenging the menopausal transition can be provides significant relief in itself; particularly for women grappling with mental health concerns.
Acceptance is often the key. Once a women knows where she is, and can connect these symptoms to menopause, she at least knows what she’s dealing with and that can be empowering. The next step is action.
Your takeaway
If you notice a deterioriation in your own mental health or in that of someone nearby, addressing these changes are critical. It may or may not be linked to menopause but, either way, seeking support from a GP and sharing how you feel is vital.
GP support is invaluable from the first menopause consultation right through the journey of change. If it transpires that mental health symptoms are not menopause-related then they still need to be dealt with. If they are menopause-related then you and your doctor can discuss your prognosis and, ongoing, any changes in symptoms, mindset and solutions.
Social support is key – sharing experiences and giving symptoms, thoughts and feelings some air time is the best way to take the power out of them, and to feel part of a common solution.
As a reminder, the content of the course belongs to The Well HQ. You have permission to access and use the content yourself or, if you are an organisation, for the number of users selected, but are not otherwise permitted to share such content with others, all in accordance with our Course Terms and Conditions.