Click play for an audio readthrough of this article
There are two families of hormonal contraceptives, let’s meet them.
Combined Contraception
(AKA the Oral Contraceptive Pill or the Combined Pill)
So-called because
It includes synthetic versions of both oestrogen and progesterone.
Administered via
A pill or a patch, or a self-inserted vaginal ring device.
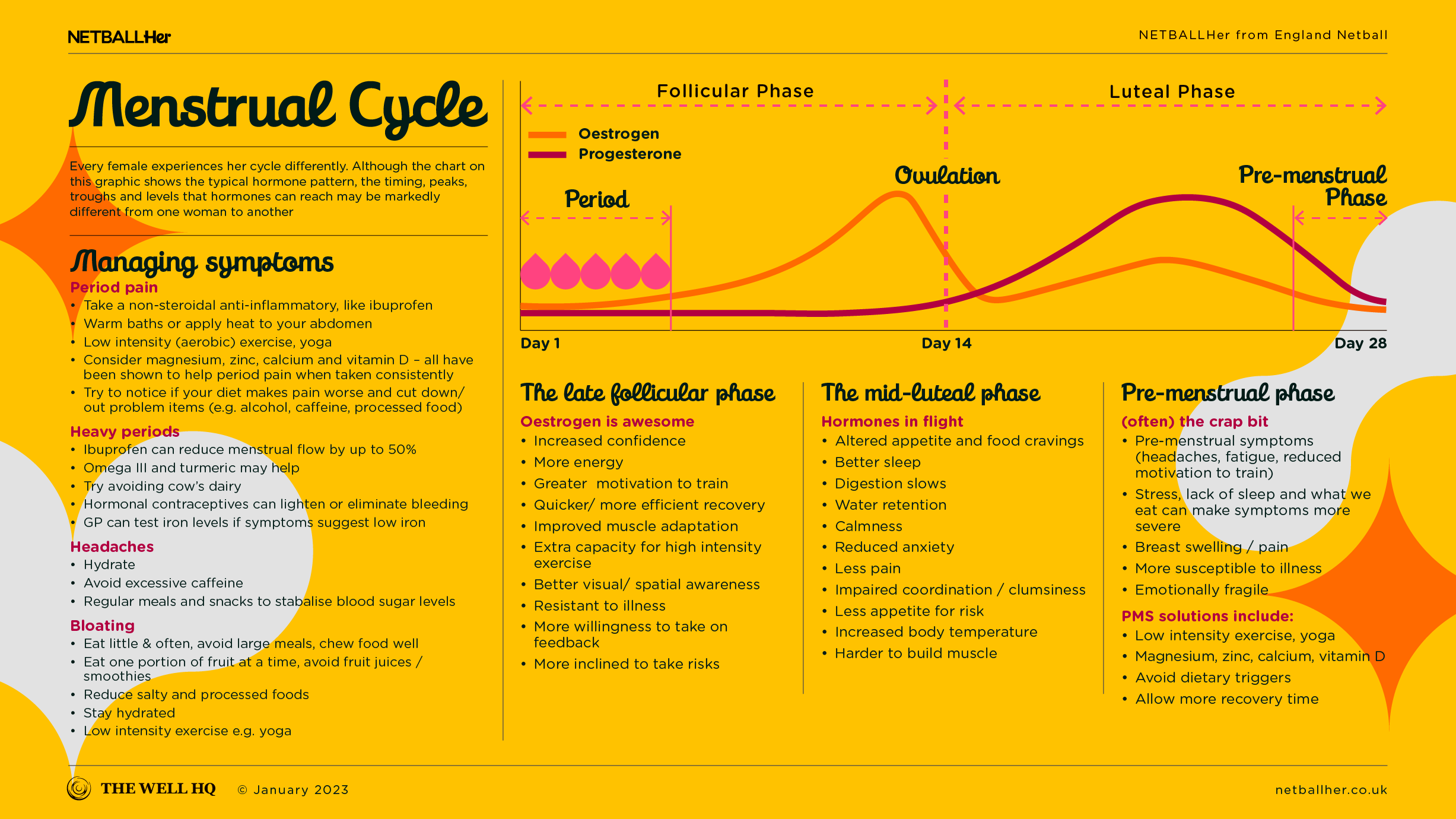
Traditionally, the combined pill (probably the most common method in the combined family) is taken for 21 days with a seven-day break. Some women take the pill continuously with no break and others take it in three month cycles; known as tricycling. All these options are safe. Taking the pill continuously means you won’t get periods at all, although some women experience what’s called ‘breakthrough bleeding’ when using this approach.
How does it help cycle symptoms?
The combined hormonal contraceptives can be used to treat heavy and painful periods, reduce premenstrual tension and ovarian cysts, and limit the risk of pelvic inflammatory disease.
Any other positives?
Some varieties of combined pill (there are more than three dozen different brands) are particularly helpful in managing conditions such as acne, endometriosis and polycystic ovarian syndrome.
There’s also evidence the combined pill can reduce the risk of ovarian and endometrial cancer.
Risks
A medical assessment is required to determine your risks and whether the combined pill will interact with any pre-existing health issues you have. The combined pill may not be suitable if, for example, you suffer migraines, smoke or have high blood pressure.
Not a period
Having a regular period is a valuable sign of wider good health, but bleeding on the combined pill is not a period – it’s a symptom of hormone withdrawal. So women using the combined pill can’t use or see their bleed as a vital sign of health – since it’s not actually a period.
So if you’re an active woman using hormonal contraception you’ll need to tune into other symptoms and red flags to alert you to underlying issues, including RED-S.
Progestogen-Only Contraception
(includes ‘fit-and-forget’ internal devices, and injections)
Like the combined options, progesterone-only products and pills can reduce monthly bleeding or stop it all together. And while that’s often welcome in the life of an athlete, eliminating the period, again, removes one of the best indicators of good (or not) general health.
However, progesterone-only forms of hormonal contraception can provide many women with relief from symptoms which impact their sport or their life.
The progesterone-only family is more diverse and common forms include:
- Pill
- Intra-Uterine Device / System (IUD / IUS)
- Implant
- Injection
Pill (AKA the ‘mini’ pill)
The progesterone-only pill is a good option for someone who suffers migraines, or another condition that’s incompatible with the combined pill.
A handful of different pharmaceutical brands produce the progesterone-only pill so the impacts can be different, pill to pill. But in general, women with heavier periods may find that their flow reduces to almost nothing, while others may still spot or experience irregular bleeds.
To remain effective as a means of birth control, this pill must be taken at roughly the same time every day, so it can be problematic for those who travel a lot or aren’t good at remembering to take medication.
IUSs
There are several different progesterone-only Intrauterine Devices, also known as Intrauterine Systems. The best-known in the UK may be the Mirena Coil, so we’ll use it as an example.
The Mirena Coil is a small plastic T-shaped device that is inserted vaginally, sits in the uterus and constantly releases a low and steady dose of progesterone. It is fitted by a medical professional and replaced every five years.
The Mirena Coil provides birth control by thickening mucus in the cervix to stop sperm from reaching or fertilising an egg. Because the Coil doesn’t suppress hormones elsewhere in the body, women with it fitted usually keep producing menstrual cycle hormones (oestrogen and progesterone) in a cyclical pattern and can even experience ovulation.
But with the Coil, those periods tend to be very light and / or very infrequent, and they may stop altogether. For these reasons, the Coil is, in some cases, used to directly treat heavy periods. It may also be used as part of hormone replacement therapy during perimenopause and menopause.
Issues
Probably the main issue with the Coil, and with IUSs more generally, is insertion: some women find the process very painful or uncomfortable, especially those who haven’t had children. The Coil is pushed through the hole in the cervix and this can prompt an intense, period-like pain that lasts for a few seconds, with cramping that may last for some hours afterwards.
But it depends on the individual. Speak to ten women who’ve had IUDs fitted and you’ll hear ten different experiences. Some feel almost nothing and others nearly pass out from the pain. There are numerous IUDs available and different brands can cater for women with a smaller or tighter cervix that can be easier to insert, and some devices last for three years instead of five.
While most IUDs can be inserted in a doctor’s surgery or sexual health clinic, they can also be inserted in your local hospital under sedation or general anaesthetic.
The most important thing here is that women should not silently endure a painful IUD procedure. If you’re in pain – please speak up. Don’t let insertion be the thing that stops you using an IUD if it is, in every other way, a great solution for you.
Implant
The implant is a small plastic rod roughly the size of a matchstick. It is inserted into the upper arm and must be replaced every three years.
The small rod contains progesterone which is gradually released (over those three years) to suppress natural hormones and stop ovulation. Like other progesterone-only methods, some women find their periods become lighter or stop entirely, while others experience infrequent spotting and / or bleeding.
Injection
There are two common types of injection, the Depo and Sayana-Press. Both are injected every three months or so, but the Depo must be administered by a nurse while Sayana-Press can be self-administered.
Women who use the injection often find their periods are lighter or stop entirely, but others may continue to bleed and/ or spot.
Research has shown that the Depo injection affects bone-mineral density, heightening the risk of bone fractures. This effect increases with longer-term use and may not be completely reversible. These risks must be outweighed by the benefits before using this approach to hormonal contraception.
As a reminder, the content of the course belongs to The Well HQ. You have permission to access and use the content yourself or, if you are an organisation, for the number of users selected, but are not otherwise permitted to share such content with others, all in accordance with our Course Terms and Conditions.