Click play for an audio readthrough of this article
Pains, discomfort, sickness, headaches, low-mood – here are strategies to develop your own unique brand of cycle resilience.
We know that some 30% of elite athletes experience heavy menstrual bleeding. And when training platform Strava and cycle app FitrWoman surveyed 14,000 active women, some 88% (basically nine out of every ten) said that symptoms negatively impacted their training at some point in their cycle.
What’s most depressing about this nine in ten stat is that many active women just accept this as their lot in life. From aspiring under-16s right up to pro athletes, we see this every day.
“It’s just how it is. It’s part of being female …”
Some do seek answers, change up their routine and maybe even see a specialist. But that’s often as far as it goes. Inevitably, a lack of progress plus embarrassment – and fear of being seen as weak or precious – sees many women back at square one. Pain and resignation …
Because it’s just our lot in life.
Switch the scenario
Imagine every month, for a few days or longer, your back spasms up and the pain is life-limiting. Imagine the pain robs you of your ability to go about daily life; to enjoy the moment; to exercise even lightly.
You’d see a doctor. You’d see a specialist. You’d leave no stone unturned in trying new strategies (stretching, swimming, posture, physio, diet, medication) to get to the root of the problem and try to turn things round.
If a bad back scenario would prompt this course of action, why are we so willing to accept the pains and limits of our menstrual cycle?
Poor knowledge in medical circles doesn’t help; neither does our lack of confidence in intimate matters. But the key reason many of us just sigh and say this is how it is …
Is because, by history and habit, this is how it is.
Take the lead
If your menstrual cycle’s holding you back, it’s time to explore strategies that make a difference.
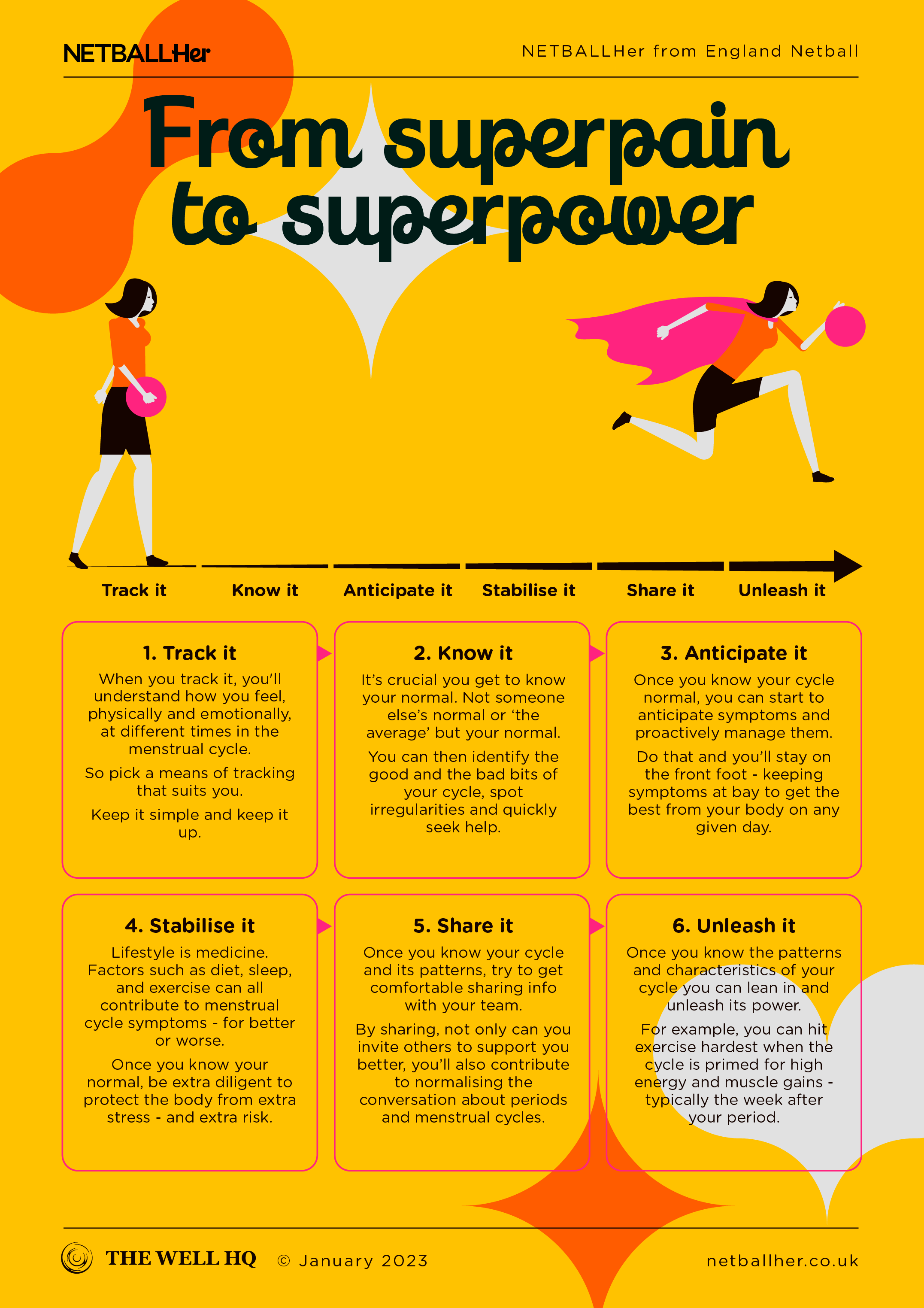
The first thing to say is that cycle tracking is a valuable and progressive step to unlock the secrets of your cycle and to start joining dots between what you do (or don’t do) and how you feel. You can’t start to effectively manage your symptoms if you aren’t clued into what they are, when they show up, and what’s happening in your life that can make them better or worse.
Rather than launching into strategies to deal with symptoms in isolation, it pays to look more generally at lifestyle … as it almost always does.
The old staples of diet, sleep, exercise and stress management are just as influential in your menstrual cycle as they are in your general health picture. For example, hormones related to stress can interfere with the healthy balance of cycle hormones, making symptoms worse. A poor diet which doesn’t give us the nutrients we need to support healthy production and processing of our cycle hormones can make symptoms more severe.
Cycle tracking (inclusive of sleep, diet and exercise data) can be a real boon in making connections between your lifestyle and menstrual symptoms.
The power pill
The pill (the hormonal contraception pill) is one of the most commonly prescribed solutions for women whose cycle / period symptoms interfere with their active life. Clinical trials show that as many as four in every five (80%) women who start the pill experience significant pain relief as a result.
Alternatively, a hormonal contraceptive coil, also known as an inter-uterine system (IUS) can be inserted into your uterus (by a GP or nurse) and will release progestin (a synthetic form of progesterone) over a five-year period. This acts both as contraception and as a means to lighten, or completely stop menstrual bleeding and pain. The IUS is often an effective treatment option in those with endometriosis).
Our article on hormonal contraception could be useful to help you decide if this approach is right for you.
Strategies for period pain
Period pain is usually caused by prostaglandins, chemicals released by the body in order to have a healthy period. Although these inflammatory chemicals are a necessary part of the process, they can cause the blood vessels and the muscles of the uterus to contract too strongly, which causes pain.
The level of prostaglandins is often highest on the first day of your period, so the pain and tummy upset tends to be more extreme at this time.
Ibuprofen / non-steroidal anti-inflammatory drugs (NSAID), such as aspirin
These over-the-counter pills work to prevent the production of excess prostaglandins. The key is to not wait until you’re doubled over before taking your pain relief. Start on the recommended dose before you even get period pain (which via tracking or a dull tummy ache you know is coming) and take it at the recommended frequency throughout the time you usually experience pain.
Note that if you’re usually heavy, ibuprofen and other NSAIDs can also lighten your flow significantly when taken throughout your bleeding days.
Heat packs
Research shows that, for some women, heat packs (hot water bottles or adhesive heat packs) are as effective as painkillers in relieving period pain.
Try pain meds and heat at once and the relief you experience can be amplified.
Yoga
Yoga twice weekly for 30 minutes, and again when period pain occurs, is shown to be effective in reducing period pain. Certain yoga poses improve blood flow to the abdomen and counter blood-flow constriction in the uterus.
So adding yoga into your schedule could alleviate symptoms enough to let you crack on with training, and with life, and there’s the extra benefit of easing stress to boost hormone health.
Acupuncture
Many active people use acupuncture to ease pain and this extends to period pains too. Research shows acupuncture is effective in alleviating inflammation, which can make cycle symptoms worse.
Strategies for disabled and neurodivergent players
As champions of Para Netball, we know the challenges that players from the disabled, deaf, blind and neurodivergent communities face.
Barriers to managing the menstrual cycle, for these groups, may go unnoticed by nondisabled people but they’re very real and can be very limiting. From inaccessible bathrooms, to sharper stigma and hygiene challenges right through to access and affordability issues when buying period products.
Asking for help can be difficult at the best of times, but it’s essential to keep an open dialogue with your club, teammates and people who support you and alert them to any specific challenges you have. It’s also worth exploring products and options beyond tampons and towels that may make managing your period easier.
For example, menstrual cups (a silicon cup in inserted into the vagina to catch blood) are cleanable and reusable and may be a more cost-effective and convenient way for you to manage your period.
Similarly, period underwear is very comfortable and it too can ease some of the practical hurdles of managing your period.
We also know bras and kit can be another challenging area so check out this article for a little more on how you, as a disabled person, can best support your breasts.
And be sure to check out Dr Emma’s videos on period management strategies and period products for more.
Trans / non-binary players
In the last section we mention period underwear, which you can find out more about here.
But period underwear, more and more, is starting to include boxer style shorts, which may be a good option for people who menstruate but don’t identify as female.
This is one facet of a shift by brands and manufacturers to be more sensitive and serve the needs of different people. In 2022 Boots joined Asda in changing in-store signage from Feminine Hygiene to Period Products, while Always has removed its longstanding brand Venus symbol to be more inclusive of trans and non-binary customers.
The market is evolving, so if you have particular needs or concerns in managing your menstrual cycle we’re in a different place now than we were even five years ago and further change is steadily coming.
Strategies for Premenstrual Syndrome (PMS)
For many women premenstrual symptoms are a normal, manageable part of the cycle. But for others, premenstrual symptoms (physical and emotional) are so significant that they interfere with daily life.
If that’s you, you may have Premenstrual Syndrome (PMS) or Premenstrual Dysphoric Disorder (PMDD). Both have their own medical diagnosis.
Roughly three in ten women experience symptoms so significant it warrants a clinical diagnosis of PMS, and about 8% of them suffer from PMDD, which is a severe PMS associated with psychiatric symptoms.
The most commonly reported PMS symptoms are headaches, migraines, breast pain, bloating, nausea, constipation, anxiety, agitation, brain fog, acne, joint pain, and trouble sleeping.
We recommend tracking your cycle as a first step to managing PMS. Via tracking you can start to understand your symptoms and patterns and any diet and lifestyle triggers. From there, exercise can help in the short term (endorphins improve mood and dampen pain) and in the long term (research shows fitter women experience less PMS than sedentary women).
Even if your pain is considerable, try to do something in the exercise family. Even if it’s just walking or yoga, it’s almost certain to help your physical or emotional symptoms.
Strategies for emotional disturbance
Whether you’ve a diagnosis or not, premenstrual symptoms can impact mood and emotion – and they can get in the way. They can hurt your confidence and motivation, as well as your relationships with others. They can leave you feeling anxious or overwhelmed, full of rage or tearful.
If you’re emotionally fragile during your cycle it’s important to recognise it and create a plan to manage it.
Your plan will be unique to you and how your emotions come out, but it may involve changing the type of exercise you do on bad days. Angry or frustrated then maybe hardcore sessions are the answer. Low mood, maybe think about your choice of workout music: something uplifting or motivating?
Premenstrual symptoms can come out in ways that upset team dynamics. If it’s not owned, the dressing room atmosphere could change: teammates may start to avoid you, or communication with your coach could break down.
So it’s best to own it, talk about it and manage it. Engage a coach or talk to your teammates about what’s going on, when it happens, why it is and what’d help. We recommend having these conversations away from the time you’re experiencing the symptoms – it can be hard to talk when you’re in the eye of the PMS storm.
Strategies for cravings, increased appetite or low energy
Some evidence suggests we become slightly more insulin resistant in the second half of the cycle. Because insulin is responsible for keeping our blood sugar levels stable, this can lead to spikes and crashes which don’t feel great; causing cravings and periods of low energy.
If you track, keep a close watch on times in the cycle when your energy and appetite levels fluctuate. At such times, try to be mindful and diligent about how and what you eat and focus on eating low-glycaemic index foods like vegetables, beans and lentils. These are foods which release energy more slowly, and avoid the sugar spikes that, say, bread and pasta cause.
It’s also important to eat regularly and don’t leave it too long between snacks and meals. This should help you maintain your energy to power your brain at work, and your body through a quality netball performance.
Strategies for tummy trouble
Gastrointestinal issues can be a big problem in the premenstrual phase, or as the period starts. Progesterone can slow your digestion and, because the body has more time to extract water from your poo, this can cause constipation. Bloating, too.
If either causes issues then stay on top of your hydration and ensure there’s plenty of fibre in your diet.
From one extreme to another, some women experience diarrhoea around this time as a result of prostaglandins causing constriction of the lower intestine. Just like with period pain, aspirin and ibuprofen block and limit prostaglandins and help to alleviate symptoms. IF taking these meds please note that both can cause irritation in the digestive tract (aspirin more so than ibuprofen) so look for pills with gastro-resistant coating.
Strategies for heavy menstrual bleeding
If you have to double up on period products, or change them every two hours or sooner, you probably have a heavy flow, just like roughly 40% of all women.
Managing heavy flow is important because heavy bleeding presents physical and emotional challenges. For one, it causes anxiety (fear of leaking, where’s the nearest bathroom?) but it also increases the risk of iron deficiency anaemia.
Active women are more at risk of iron deficiency anaemia. Because exercise ruptures red blood cells, that plus a heavy period bleed is a double-whammy which can result in symptoms such as fatigue, breathlessness, and light-headedness.
If you think you’re low on iron then get your levels checked by a doctor before doing anything else. Don’t dive head first into supplements if you don’t need to because too much iron could result in constipation, nausea and pain.
Strategies for breast pain
Breasts tend to change across the menstrual cycle. Week to week, they may become enlarged, or sore, or lumpy. The first thing to say is that you need to know your own normal so you can identify lumps that aren’t cyclical and shouldn’t be there.
For some 70% of women, breast pain is part and parcel during certain points of the menstrual cycle. And of those who suffer, 20% say the pain is moderate to extreme.
Regular and predictable breast pain may seem like an annoying thing you just have to grit your way through, but too few women think about treating the pain with better breast support.
Research shows that a well-fitting, supportive bra can improve breast pain by up to 85%. It sounds so simple (and in many ways it is) but your well-fitting bra may need to accommodate changes in your breast size and shape. It could be that you need a different bra (shape or size) at different times of your cycle.
Strategies for premenstrual magnification
Premenstrual magnification is when issues you already suffer from (for example, irritable bowel syndrome, acne, migraines or asthma) attack with a vengeance in the premenstrual phase of the cycle.
These seem like PMS symptoms but they’re not, exactly. They are a manifestation of an underlying problem that flares up under PMS conditions. The strategy here is to try to get to the underlying condition, most likely through medical help and support, and find ways to better treat and / or manage that.
Strategies for planning ahead
Habit cues are your ability to recognise when a particular part of your cycle is coming up and what it’s going to throw at you. You might feel changes physically or emotionally, or you might be tracking your cycle and know what’s coming down the line.
For example, you may have learned that you always feel a rush of positivity in the week after your period. So why not get out and exercise that week and put all that awesome oestrogen to work.
Or maybe you know the initial signs of premenstrual symptoms. When those start it could be a cue for you to go into pain management mode. Maybe it’s also a cue for you to engage more in things you enjoy (music, walks, baking, yoga) to get a headstart in countering the low mood that often accompanies this phase.
Start using those body and mood cues to prepare yourself for what comes next and take the actions that’ll ensure you stay on top.
As a reminder, the content of the course belongs to The Well HQ. You have permission to access and use the content yourself or, if you are an organisation, for the number of users selected, but are not otherwise permitted to share such content with others, all in accordance with our Course Terms and Conditions.