Click play for an audio readthrough of this article
Hormonal, non-hormonal and lifestyle solutions can all ease menopause symptoms – here’s the lowdown.
Introduction
Every woman is different and every menopause experience is different. A woman’s individual needs, wants and risk profile need to be taken into account when exploring treatment and solutions, and the approach needs to be holistic.
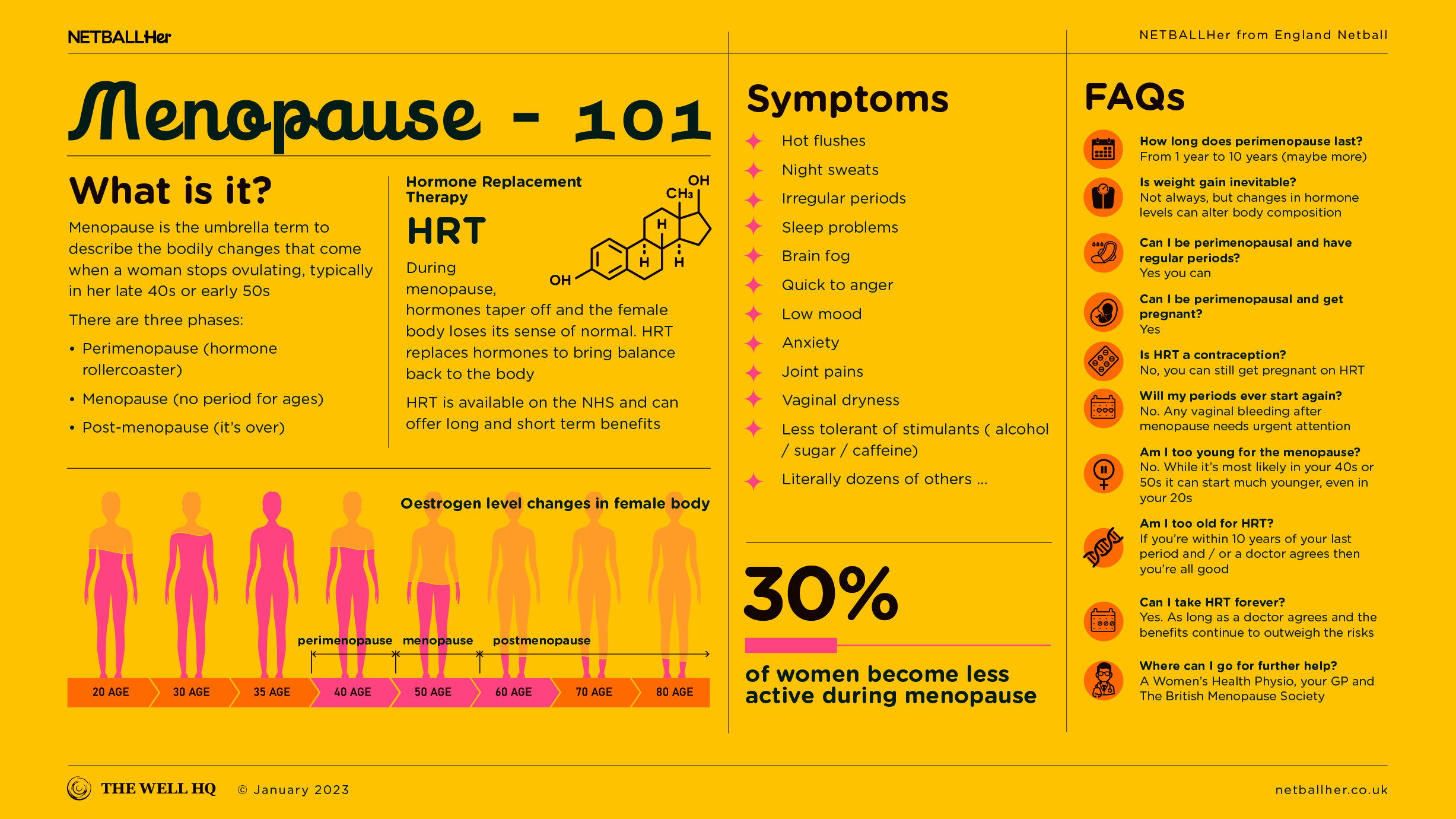
Hormone Replacement Therapy (HRT) is first line treatment, as per The National Institute for Health and Care Excellence, or NICE, for perimenopausal symptoms, as it offers both short term and long term benefits.
But HRT is not the beginning and end of it. Some women won’t, can’t or don’t need to take HRT, and other treatment options are available. Non-hormonal medications can also help to ease symptoms, and lifestyle is absolutely fundamental.
Exercise, diet, stress management, sleep … addressing these things can help hugely in managing menopause symptoms. Similarly, talking therapies, yoga, supplements, complementary medicines, and/ or a combination of all of the above may be for you.
The important thing is to consult the right experts and put yourself and your needs first.
What is HRT and how does it help?
Throughout life the female body relies on hormones to keep a sense of rhythm and order. During menopause, those hormones go into decline via a chaotic journey south, leaving the body confused and without its old sense of normal.
HRT replaces those key hormones to bring balance back to the body. The most recent HRT treatments are what’s called ‘body identical’, meaning they’re almost identical to the hormones women produce naturally. That means the body tolerates HRT well.
HRT is currently available on the NHS and offers a range of benefits. It can quickly ease symptoms in the short term, and promote healthier bones, hearts, bowels, skin and brain over a longer timeline.
How do you take HRT?
Under medical supervision!
HRT can be systemic, which means it travels via the bloodstream through the whole body, or it can be localised, which means it focuses on a small area of the body – the vagina for example.
Systemic
This is HRT into the bloodstream, usually via the stomach (a tablet) or absorbed through the skin (transdermal). Transdermal HRT includes things like patches, gels, sprays and creams. This method of HRT should ease menopausal symptoms and it will have long term benefits elsewhere in the body.
Localised
Also called topical HRT, this includes vaginal gels, creams, and vaginal rings (to be inserted into the vagina). The genital area is rich in oestrogen receptors so when oestrogen levels drop it becomes an epicentre for symptoms such as dryness, itching, soreness or recurrent urinary tract infections.
These symptoms are also common after the menopause (roughly 80% of women experience them) and can worsen with time. Sadly, such conditions often go untreated or undertreated so education and awareness is key to avoid women suffering unnecessarily.
Vaginal oestrogen is very low risk (it’s the equivalent of 1 HRT tablet across a whole year) and it can be very effective. In fact, nowadays it’s even available over-the-counter.
But do remember: menopause impacts different women differently so so consult a good woman’s health GP to understand your options for your symptoms.
HRT risks and objections
HRT is today the first line treatment for menopause symptoms, as promoted by NICE – the UK body that writes our medical guidelines. There are risks (see below) in taking it, and whether you can or not depends on multiple health and lifestyle factors, hence why it’s so important to consult a doctor.
Modern HRT mimics natural hormones incredibly well and is life-changing for some women, yet others don’t like the idea of chemical hormones in their body and want to try a different approach to managing symptoms. Although HRT is the first line treatment, it’s not mandatory and it’s not the only way to deal with menopause symptoms and stay healthy in midlife and beyond.
Interestingly, HRT still makes some people – including some doctors – uneasy, and this is a hangover from some poor science communication about 20 years ago, when an influential (but misleading) paper came out and concluded that HRT caused “significant risks” of breast cancer, heart disease and other life-changing conditions.
But this study was later described as “melodramatic” and revised. Subsequent studies have consistently demonstrated that, with the right clinical support, hormone replacement therapy is a safe and viable treatment for the menopause.
What else is there apart from HRT?
Not everyone can or wants to take HRT, and there are other approaches to explore which offer women relief. For example, doctors may prescribe forms of antidepressants and other non-hormonal alternatives to help with symptom control.
Research has shown that the majority of menopausal women are deficient in magnesium and vitamin D, so many find that supplementing with these micronutrients helps to alleviate symptoms.
On the longlist of other supplements some women turn to are black cohosh, red clover and sage. While there’s no evidence to suggest these make any difference, our philosophy is this …
If it helps it helps. If it’s safe to use, go for it.
What else can I do?
There are of course practical solutions to deal with specific menopause symptoms.
For hot flushes you can review your bedroom temperature and shop for clothing that helps keep you cooler; breathable materials, for example, such as cotton, linen, or jersey.
Often it’s not actually the hot flush itself but the cold-sweat-shivers that disrupt sleep most. Some innovative clothing is now available to help remove sweat from the skin and enable you to regulate your body temperature at night. Check out https://www.becomeclothing.com/
For itching and pain during sex, vaginal oestrogen (via pessaries, cream or a vaginal ring) can help, as can lubricants and vaginal moisturisers such as Sylk or Yes!.
Given the emotional rollercoaster that is the perimenopause, counselling, CBT and other therapies can be massively helpful during a hyper-stressful and confusing time in a woman’s life.
Then there’s exercise and lifestyle. This article explains how staying active is a massive boon to your health, wellbeing, symptoms and sleep during midlife.
As a reminder, the content of the course belongs to The Well HQ. You have permission to access and use the content yourself or, if you are an organisation, for the number of users selected, but are not otherwise permitted to share such content with others, all in accordance with our Course Terms and Conditions.