Click play for an audio readthrough of this article
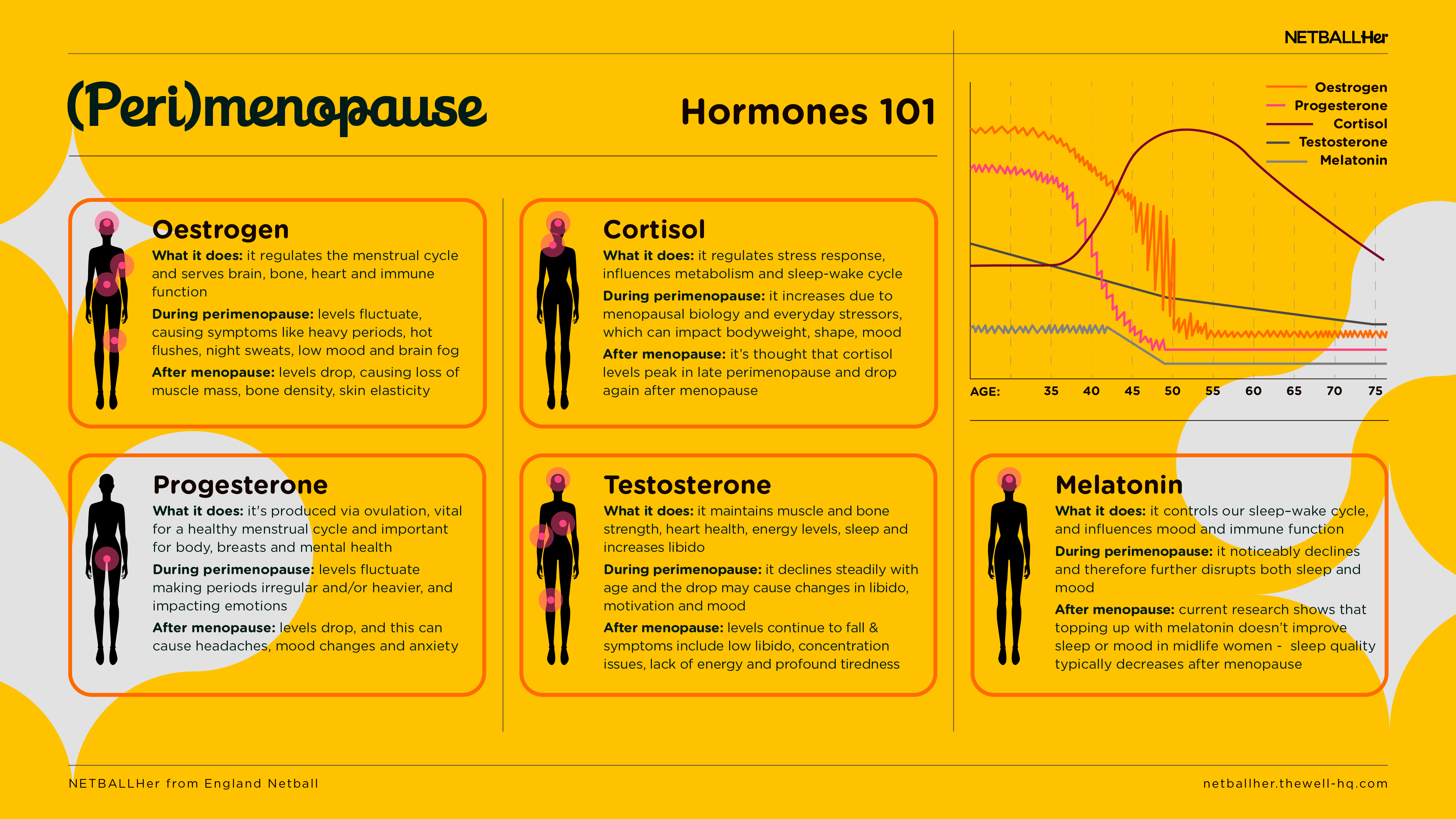
In a nutshell, the female body has gotten used to a certain chemical normal. It’s gotten used to certain hormones arriving in a certain pattern … and that’s been the norm for 30-ish years.
But in perimenopause that pattern goes haywire. The hormones of the cycle rollercoaster up and down and, eventually, levels dwindle. This causes disruption throughout the body – so cue a range of physical, mental and emotional symptoms.
Let’s meet the hormones.
Oestrogen
In your fertile years oestrogen is not only important for regulating the menstrual cycle, but it is also vital for the health of so many other systems in our body. Brain, bone, cardiovascular and immune health, to name a few. It also supports the release of serotonin – the good mood hormone.
During your fertile years, the second week of the menstrual cycle (give or take) is when oestrogen hits its peak. The influence of oestrogen can mean you feel bulletproof, motivated and ready to take on the world.
Into perimenopause, oestrogen levels are ultimately heading south but on that journey they can reach all-time-peaks often followed by big crashes. The sense of confidence and vigour that oestrogen used to push also fades during this time.
All this without the good-mood boost of serotonin and it’s no wonder that low mood, anxiety and confusion are symptoms synonymous with perimenopause.
Oestrogen is an important hormone for helping build up the lining of the uterus during the menstrual cycle (in case we get pregnant and want to implant an embryo in there), and this lining is shed each month AKA the period. During perimenopause the erratic upward swings in oestrogen can mean that lining is built up more than ever before, and heavy or ‘super’ periods can be a feature of some women’s perimenopause.
Then there’s symptoms directly related to low levels of oestrogen, such as hot flushes, vaginal dryness, brain fog and the increased likelihood of leaking due to oestrogen being less available to support pelvic floor and bladder functioning.
The decline in oestrogen during perimenopause can affect each individual in very different ways: some women are more sensitive to these changes in hormone levels than others, meaning some women sail through with no symptoms while others suffer a smorgasbord of symptoms, including mental health symptoms which are often an early menopause tell-tale.
Progesterone
During your fertile years, progesterone wants the body to relax and de-stress. It is released only after we have ovulated, and levels rise in the third week (or so), typically making women calmer and more risk-averse.
In perimenopause, progesterone winds down and takes with it those sleep-promoting mechanisms, our calmness and the desire to relax. Hence why perimenopause is associated with emotional traits such as irritability, low mood, overwhelm and anxiety, which can all be exacerbated by a lack of sleep.
As we ovulate less and less, we produce less progesterone and our cycles can become less regular, with three, six or even ten month gaps in between. It’s not until there is a year since the last period that a woman transitions from perimenopause into menopause.
Testosterone
Primarily thought of as a male hormone – because it’s produced in high levels in the male body – testosterone is a key hormone that powers a female’s sex-drive and supports her cognitive function, motivation and confidence, and builds bone and muscle strength.
The decline of testosterone during menopause is actually just coincidence … it’s an age thing. It has been slowly tapering off since early adulthood.
Nonetheless, falling testosterone combined with other hormone activity can compound some of the emotional and physical impacts of perimenopause. A lack of sex-drive, low mood, lost motivation, weight gain, and age-related muscle and bone weakness are known effects of low testosterone.
Cortisol
Cortisol is the stress hormone and there’s more of it in midlife as a result of the body’s changing chemistry plus the everyday stressors of a busy life.
Cortisol is essential to our health: it’s what kick-starts us in the morning and gives us the energy to get out of bed. But cortisol levels should naturally decline over the day. If instead levels are higher or lower than normal for prolonged periods, it can compromise a woman’s wellbeing.
Light exercise, breath work and doing activities where you are in the moment (as opposed to multi-tasking – which we’re all total queens at) are good ways to counter stress during perimenopause.
Note that exercise causes stress in the body, which is a healthy and normal response. But in midlife, when our body is already high on biological and psychological stress, we need to bookend training with great warm ups and brilliant cool downs to help our body manage, stay healthy and not get overloaded. This is one of several non-negotiables … so click here for more.
As a reminder, the content of the course belongs to The Well HQ. You have permission to access and use the content yourself or, if you are an organisation, for the number of users selected, but are not otherwise permitted to share such content with others, all in accordance with our Course Terms and Conditions.